Medical and Complementary Therapies
In addition to self-care practices that you can do to help reduce pain, you may find that you require other therapies which are provided by professionals.

What other medical and complementary therapies can help me with my pain?
Massage therapy
Massage therapy is cheaper than physiotherapy and can give short term pain relief by working on specific, painful muscle groups.
To find out more please contact a member of the Health and Wellbeing team, on 01480 474074 or email, if you want help finding a massage therapist.
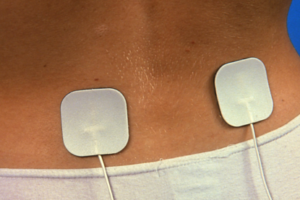
Tens machines
A TENS Machine stands for Transcutaneous Electric Nerve Stimulation machine. It’s a small battery-operated machine which sends electrical impulses into your body.
There are different theories about how it works. One theory is that it helps to block pain messages been sent to your brain. Another theory suggests they help release feel good hormones called endorphins which can also help block pain signals.
Although the evidence to say they work is mixed, some people do find them very helpful.
Acupuncture
Acupuncture is a form of treatment that involves inserting very thin needles through a person's skin at specific points on the body to various depths. There is some evidence that it can help relieve pain.
Some beneficiaries find acupuncture helpful for chronic pain.
You can find an acupuncturist here
What Medication can I take for Pain?
Painkillers
Painkillers such as Paracetamol or anti-inflammatory drugs like Ibuprofen or Naproxen can be used to treat the symptoms of pain.
Your GP can advise you about the kinds of painkillers that will suit you best. Your pharmacist can also advise you. They can cause irritation of the stomach and can’t be used if you’ve had a history of bleeding or ulcers in the gut. If you are using painkillers continuously to cope with everyday life, ask about other things you can do to cut down how many you take.
Speak to your GP or one of the Medical Advisers at the Trust if you’re unsure.
You can read more about anti-inflammatory drugs here:
The NHS provides information on Non-steroidal anti-inflammatory drugs (NSAIDs) which may be used to treat causes of long term pain.
The British Pain Society also provides detailed information on NSAIDs.
Opioids
Opioids may be offered if your pain is causing you significant problems. These vary in strength and will be carefully considered and supervised by your doctor, as they can be habit-forming. They tend to work best for acute episodes of pain, so when you have a pain flare up.
They are not necessarily the best option for chronic (every day) pain.
Codeine is the weakest opioid, Tramadol is of medium strength, and Morphine and Oxycodone are the strongest opioids. They can cause constipation so please speak to your GP or pharmacist if this happens.
If you can’t take oral medicine (tablets or syrup) you may be offered medicines in the form of creams, gels or patches. These are often just as effective as tablets and treat the area where they have been applied without affecting other parts of your body.
Other pain medications for Chronic Pain
Pain medication is used in cases of complex, chronic pain. Your GP will tell you the best drugs to take and will check your progress regularly; starting with a low dose of a weak drug which can be increased or changed until you have the best pain relief for you. Your doctor will also explain any possible side-effects to you.
It’s really important to discuss your symptoms regularly, and any side-effects you experience. This includes your mood, sleep and how you’re feeling in general.
If side-effects are problematic you may need to reduce or stop taking your medication. Your doctor will suggest alternatives. Sometimes you will continue to take your medication alongside the new one, to keep your pain under control whilst you make the switch.
Read more about types of medication used in chronic pain, such as Amitriptyline, Gabapentin or Pregabalin:
Injections
Injections can also help with pain. Local anaesthetic, sometimes combined with a steroid, can help in the short term and may need to be repeated at intervals.
The NHS have produced a document to give more information on injection treatments.
Longer term results can be gained from ‘denervation’ injections which partially destroy the nerves causing your pain.
There is also a NHS document on the ‘denerving’ treatment for further information.
Pain clinics
If your pain is resistant to treatment offered by your GP or you are finding that your pain is stopping you doing the activities you enjoy, you can ask to be referred to a pain clinic. Pain clinics aim to look at your pain holistically and treatments may include:
- medicine
- pain-relief injections
- manual therapy
- exercise
- TENS machines
- complementary therapy
- psychological therapy
Pain Management Programmes
If you attend a pain clinic, you may be offered something called a pain management programme (PMP).
A PMP aims to improve the quality of your life whilst learning to live with the pain you experience.
A PMP usually means attending group sessions with other people who experience chronic pain. The sessions may include:
- gentle movement
- relaxation exercises such as breathing exercises and mindfulness
- dealing with emotions and mood
- group discussion
- techniques such as pacing
Surgery
Surgery is sometimes an option in managing pain. You can ask your GP to refer you for a second opinion from a surgeon who can advise you on how surgery may help.
Some final tips….
Taking a look at your situation and what might be contributing to your pain and doing something about it can really help. Asking yourself some key questions is a good start: –
- Are you relying heavily on painkillers when you could cut down?
- Are there lifestyle changes you could make such as, losing weight, improving your diet or quitting or reducing smoking and alcohol intake?
- Have you got the right balance of exercise and relaxation or inactivity?
- Can you make changes to your posture and movement when doing everyday tasks (for example, using a computer, driving) that can reduce the strain on your body?
- Are there stresses and strains in your life that could be affecting your ability to sleep or relax, and putting added strain on your body?
Further information and support
If you want some more advice on what you’ve read, or want to speak about your situation, then please contact a member of the Health and Wellbeing team on 01480 474074, or email.
There's lots of self-help advice available from a variety of organisations supporting people living with long-term pain, such as:
Action on Pain
British Pain Society
Pain Concern
PainSupport