Working Together To Live With Pain
 Understanding what's behind persistent pain and learning some self-care skills so you can enjoy life
Understanding what's behind persistent pain and learning some self-care skills so you can enjoy life
Carolyn Desforges recently attended a public lecture on pain by Paul Chazot (Neuro-pharmacologist) from The Pain Challenge Academy and Dr. Frances Cole (GP) at the Wolfson Research Institute for Health and Wellbeing, Durham University. As over 90% of the beneficiary community are living with some type of pain, this topic is very relevant to those living with thalidomide damage.
The Wolfson Institute has multidisciplinary teams working on understanding the symptoms of pain, how we perceive and experience it, as well as researching the application of medical/pharmacological interventions and social mediations in managing pain. It is now accepted that many current pain medications not only have limited use, but also have serious safety concerns.
Persistent pain and the Pain Cycle
Persistent pain cannot be ‘fixed’ or ‘cured’. To help manage it, there needs to be an understanding of an individual’s experience and an individually tailored programme to help manage it. Health care professionals also realise they need to change how they engage with people with persistent pain.
However, whilst it is most helpful to have support in managing persistent pain, there are also ways which we can start to understand our own pain, and begin to think about our own ways of self-managing our pain.
First of all it is important to understand what is behind our pain, before beginning to manage it. The aim is to move from the pain cycle to a self-care cycle.
The Pain Cycle - It's a mix of bio-psycho-social issues
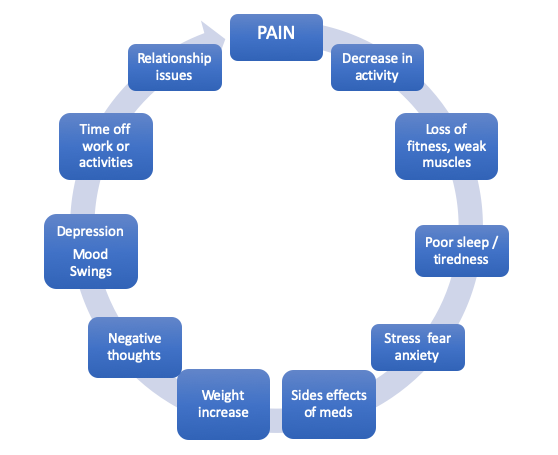
The cycle starts with Pain which leads to the following issues:
- Decrease in activity
- Loss of fitness, weak muscles
- Poor sleep/tiredness
- Stress, fear, anxiety
- Side effects of medication
- Weight increase
- Negative thoughts
- Depression, mood swings
- Time off work or activities
- Relationship issues
Changing the impact of pain - The Self-Care Cycle
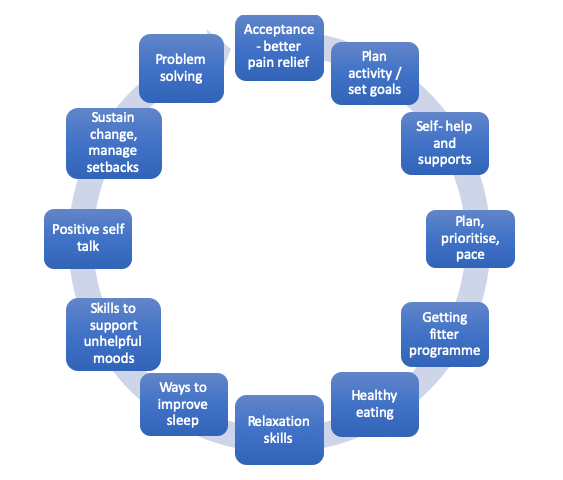
The cycle starts with Acceptance and better pain relief which leads on to:
- Plan activities and set goals
- Self-help and supports
- Plan, prioritise, pace
- Getting fitter programme
- Healthy eating
- Relaxation skills
- Ways to improve sleep
- Skills to support unhelpful moods
- Positive self-talk
- Sustain change, manage setbacks
- Problem solving
So how can we learn to manage pain? Understanding Pain and the Brain
Our brain draws on our brain memories but the system becomes oversensitive and can give us an inaccurate interpretation. Persistent pain is very different from the kind of pain you experience when you injure yourself. It goes on long after the original damage has healed – it's as if the brain can no longer 'turn down the volume'. Reducing persistent pain involves retraining your brain. If we can figure out what is going on, we can then understand some changes that can help us manage the pain.
The 10 Footsteps
 In Darlington, County Durham, a chronic pain management programme using a 'Skills not Pills' approach, has supported GPs, clinicians and pharmacists to implement a self-management programme to reduce pain, alongside implementing safe prescribing.
In Darlington, County Durham, a chronic pain management programme using a 'Skills not Pills' approach, has supported GPs, clinicians and pharmacists to implement a self-management programme to reduce pain, alongside implementing safe prescribing.
The programme is called the 10 Footsteps Approach and you can read more about it on the Live Well With Pain website.
It is important that we 'care' for ourselves, moving from enduring life to enjoying life.
The 10 footsteps are:
- Understanding how your brain is interpreting pain.
- Acceptance. This is not about giving in, but changing your focus towards what you want to do with your life – learning to manage the pain.
- Pacing. This is one of the key self-management skills for people living with persistent pain. Changing your pacing style could bring many benefits and lessen your pain.
- Setting goals. Having goals helps you to focus on the things that matter most to you – you must not forget to build in some rewards.
- Get more active. People with pain find it helps to be more active even if it wasn't part of their life before pain. Getting support here to maintain motivation is key.
- Managing moods. It is normal to struggle with moods when you have persistent pain. There are many ways to lessen the stress or pressure you're under. It is managing to discover which ones work best for you and then use them often.
- Sleep. Lots of people with pain have difficulties sleeping, but making some changes to what you do during the day will help you sleep better – this includes what you eat and drink, your night-time routine, and having a ‘fit for sleep’ bedroom.
- Food, relationships and work. Eating well, doing things with other people, and going back to work, or other retirement activities gives life routine, structure and purpose.
- Relaxation and mindfulness. These can lessen pain levels, reduce stress and improve concentration.
- Managing setbacks. People with pain experience setbacks for many reasons – and sometimes for no obvious reason at all. Having a setback plan ready can help you get back on track sooner – it is important to stay kind to oneself during these times.
Additional Resources
There are some excellent resources to help support our self-management of pain. Trust medical advisers and Health & Wellbeing staff can also offer support. Wishing you all the best for your self-care and a more enjoyable life less dominated by pain!
Understand Pain
from Live Well With Pain

Pain Information
from Dr Susan Brennan

