Pain
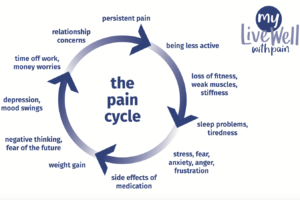
We have all experienced pain and know it as an unpleasant sensation, but degrees of pain can vary from the mild to the severe, acute (short-term) to the chronic (persisting). For many people living with thalidomide damage, pain can become part of life, often made worse by every-day activities like driving, housework or using a computer.
Trust Medical Adviser, Dr Susan Brennan, explains what pain is, how it can affect us and what self-care we can do to help manage pain. In addition she discusses medical and complementary therapies available to combat pain. You can read the information on our website or watch her on video.
Additional Information and Support Organisations
BSL health information
BSL video health information on chronic pain is available from NHS Scotland. Most of the information is relevant to anyone in the UK, but please note there may be some Scotland specific pathways where you will need to find the alternative for the country you are in.
Watch BSL video on chronic pain (NHS Scotland)